Abstract
Background
Innovative technologies challenge healthcare systems, as evidence on costs and benefits frequently usually are slow to reflect new technology. We investigated these dynamics for Germany, using the emergence of transcatheter aortic valve implementation (TAVI) as an alternative to conventional aortic valve replacements (CAVR).
Objective
We focused on the role of patient co-morbidity—which would be a medical explanation for adopting TAVI—and hospital ownership status, hypothesizing that for-profit facilities are more likely to capitalize on the favorable reimbursement conditions of TAVI.
Methods
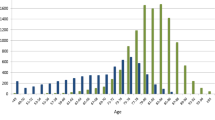
The analysis uses claims data from the Techniker Krankenkasse, the largest health insurance fund in Germany, for the years 2009–2015, covering 2892 patients with TAVI and 9523 with CAVR. The decision on TAVI versus CAVR was estimated for patient-level data, that is, socioeconomic data as well as co-morbidity. At the hospital level, we included the ownership type. We also controlled for effects of the respective owner (rather than the type of ownership), including a random intercept.
Results
While the co-morbidity score of TAVI patients was much higher in the early years, over time, the score almost converged with that of CAVR patients. This is in agreement with emerging evidence that suggests the use of TAVI also leads to better patient outcomes. Our results indicate that the type of ownership does not drive the switch to TAVI. We found little, if any, effect from the respective owner, regardless of ownership type.
Conclusion
Overall, the effects of co-morbidity suggest that providers acted responsibly when adopting TAVI while evidence was still emerging.

Similar content being viewed by others
References
IQTIG: Qualitätsreport 2015 [Quality report 2015]. Berlin. 2016.
Kuck K-H, Eggebrecht H, Elsässer A, Hamm C, Haude M, Ince H, Katus H, Möllmann H, Naber CK, Schunkert H, Thiele H, Werner N. Qualitätskriterien zur Durchführung der kathetergestützten Aortenklappenimplantation (TAVI). Der Kardiologe. 2016;10(5):282–300. https://doi.org/10.1007/s12181-016-0082-4.
Miller DC, Blackstone EH, Mack MJ, Svensson LG, Kodali SK, Kapadia S, Rajeswaran J, Anderson WN, Moses JW, Tuzcu EM, Webb JG, Leon MB, Smith CR. Transcatheter (TAVR) versus surgical (AVR) aortic valve replacement: occurrence, hazard, risk factors, and consequences of neurologic events in the PARTNER trial. J Thorac Cardiovasc Surg. 2012;143(4):832–43. https://doi.org/10.1016/j.jtcvs.2012.01.055.
Adams DH, Popma JJ, Reardon MJ. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014;371(10):967–8. https://doi.org/10.1056/nejmc1408396.
Fairbairn TA, Meads DM, Hulme C, Mather AN, Plein S, Blackman DJ, Greenwood JP. The cost-effectiveness of transcatheter aortic valve implantation versus surgical aortic valve replacement in patients with severe aortic stenosis at high operative risk. Heart. 2013;99(13):914–20. https://doi.org/10.1136/heartjnl-2013-303722.
Indraratna P, Ang SC, Gada H, Yan TD, Manganas C, Bannon P, Cao C. Systematic review of the cost-effectiveness of transcatheter aortic valve implantation. J Thorac Cardiovasc Surg. 2014;148(2):509–14. https://doi.org/10.1016/j.jtcvs.2013.10.023.
Mollmann H, Bestehorn K, Bestehorn M, Papoutsis K, Fleck E, Ertl G, Kuck KH, Hamm C. In-hospital outcome of transcatheter vs. surgical aortic valve replacement in patients with aortic valve stenosis: complete dataset of patients treated in 2013 in Germany. Clin Res Cardiol. 2016;105(6):553–9. https://doi.org/10.1007/s00392-016-0962-4.
Schindel R. Qualitätsaspekte der kathetergestützten Aortenklappenimplantation. Welt der Krankenversicherung. 2012;6/2012:192–4.
Roeder N, Bunzemeier H, Heumann M. Das KHSG und seine potenziellen Auswirkungen auf die Leistungsvergütung der Krankenhäuser. Das Krankenhaus. 2015;7.2015:626–35.
Horwitz JR. Making profits and providing care: comparing nonprofit, for-profit, and government hospitals. Health Aff (Millwood). 2005;24(3):790–801. https://doi.org/10.1377/hlthaff.24.3.790.
Bayindir EE. Hospital ownership type and treatment choices. J Health Econ. 2012;31(2):359–70. https://doi.org/10.1016/j.jhealeco.2012.01.003.
Sloan FA. Not-for-profit ownership and hospital behavior. In: Culyer AJ, Newhouse JP, editors. Handbook of health economics, vol. 1B. Amsterdam [u.a.]: Elsevier [u.a.]; 2000. p. 1141–74.
Barros PP, Siciliani L. Public and private sector interface. In: Pauly MV, Mcguire TG, Barros PP, editors. Handbook of health economics 2, vol. 2012. Amsterdam: Elsevier, North Holland; 2011. p. 927–1001.
Horwitz JR, Hsuan C, Nichols A. The role of hospital and market characteristics in invasive cardiac service diffusion. Rev Ind Organ. 2018. https://doi.org/10.1007/s11151-018-9625-0 (First online 23 Mar 2018).
Horwitz JR, Nichols A. Hospital ownership and medical services: market mix, spillover effects, and nonprofit objectives. J Health Econ. 2009;28(5):924–37. https://doi.org/10.1016/j.jhealeco.2009.06.008.
Burke DE, Wang BB, Wan TT, Diana ML. Exploring hospitals’ adoption of information technology. J Med Syst. 2002;26(4):349–55.
Lin SC, Everson J, Adler-Milstein J. Technology, incentives, or both? Factors related to level of hospital health information exchange. J Med Syst. 2018;26:349–55. https://doi.org/10.1111/1475-6773.12838.
Tiemann O, Schreyögg J, Busse R. Hospital ownership and efficiency: a review of studies with particular focus on Germany. Health Policy. 2012;104:163–71. https://doi.org/10.1016/j.healthpol.2011.11.010.
Karmann A, Roesel F. Hospital policy and productivity—evidence from German states. Health Econ. 2017;26(12):1548–65. https://doi.org/10.1002/hec.3447.
Schmid A, Ulrich V. Consolidation and concentration in the German hospital market: the two sides of the coin. Health Policy. 2013;109(3):301–10. https://doi.org/10.1016/j.healthpol.2012.08.012.
Clark MA, Arnold SV, Duhay FG, Thompson AK, Keyes MJ, Svensson LG, Bonow RO, Stockwell BT, Cohen DJ. Five-year clinical and economic outcomes among patients with medically managed severe aortic stenosis: results from a Medicare claims analysis. Circ Cardiovasc Qual Outcomes. 2012;5(5):697–704. https://doi.org/10.1161/circoutcomes.112.966002.
Abildstrøm SZ, Hvelplund A, Rasmussen S, Nielsen PH, Mortensen PE, Kruse M. Prognostic information in administrative co-morbidity data following coronary artery bypass grafting. Eur J Cardiothorac Surg Off J Eur Assoc Cardiothorac Surg. 2010;38(5):573–6. https://doi.org/10.1016/j.ejcts.2010.03.007.
Guo G, Zhao H. Multilevel modelling for binary data. Am Rev Sociol. 2000;26:441–62.
Schabenberger O. Introducing the GLIMMIX procedure for generalized linear mixed models. In: Proceedings of the 30th annual SAS users group
Dai J, Li Z, Rocke D. Hierarchical logistic regression modeling with SAS GLIMMIX. Davis: University of California; 2006.
Zhu M. Analyzing multilevel models with the GLIMMIX procedure. Paper SAS026-2014. Cary, NC: SAS Institute Inc; 2014.
Gemeinsamer Bundesausschuss: Beschluss des Gemeinsamen Bundesausschusses über eine Richtlinie zu minimalinvasiven Herzklappeninterventionen: Erstfassung. Bundesanzeiger BAnz AT 24.07.2015 B6; 2015.
Neubauer S, Kreis K, Klora M, Zeidler J. Access, use, and challenges of claims data analyses in Germany. Eur J Health Econ. 2017;18:533–6. https://doi.org/10.1007/s10198-016-0849-3.
Author information
Authors and Affiliations
Contributions
Udo Schneider was responsible for the study design, the statistical analysis, and the preparation of the manuscript draft. Andreas Schmid prepared data for hospital ownership and contributed to the statistical analysis, literature review, and the final manuscript. Roland Linder was responsible for the medical setting of the study and critical assessment of the statistical analysis. Dirk Horenkamp-Sonntag designed the pick-up of the diagnoses for the co-morbidity index and its interpretation. Frank Verheyen was responsible for study design and study co-ordination.
Corresponding author
Ethics declarations
Conflict of interest
No funding was received for the study. Udo Schneider, Andreas Schmid, Roland Linder, Dirk Horenkamp-Sonntag, and Frank Verheyen declare that they have no conflicts of interest.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schneider, U., Schmid, A., Linder, R. et al. The Choice of Transcatheter Aortic Valve Implementation (TAVI): Do Patient Co-morbidity and Hospital Ownership Type Matter?. Appl Health Econ Health Policy 16, 735–744 (2018). https://doi.org/10.1007/s40258-018-0414-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-018-0414-6