Abstract
Background
The current draft of the German Hospital Structure Law requires remuneration to incorporate quality indicators. For neurosurgery, several quality indicators have been discussed, such as 30-day readmission, reoperation, or mortality rates; the rates of infections; or the length of stay. When comparing neurosurgical departments regarding these indicators, very heterogeneous patient spectrums complicate benchmarking due to the lack of risk adjustment.
Objective
In this study, we performed an analysis of quality indicators and possible risk adjustment, based only on administrative data.
Methods
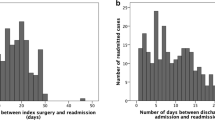
All adult patients that were treated as inpatients for a brain or spinal tumour at our neurosurgical department between 2013 and 2017 were assessed for the abovementioned quality indicators. DRG-related data such as relative weight, PCCL (patient clinical complexity level), ICD-10 major diagnosis category, secondary diagnoses, age and sex were obtained. The age-adjusted Charlson Comorbidity Index (CCI) was calculated. Logistic regression analyses were performed in order to correlate quality indicators with administrative data.
Results
Overall, 2623 cases were enrolled into the study. Most patients were treated for glioma (n = 1055, 40.2%). The CCI did not correlate with the quality indicators, whereas PCCL showed a positive correlation with 30-day readmission and reoperation, SSI and nosocomial infection rates.
Conclusion
All previously discussed quality indicators are easily derived from administrative data. Administrative data alone might not be sufficient for adequate risk adjustment as they do not reflect the endogenous risk of the patient and are influenced by certain complications during inpatient stay. Appropriate concepts for risk adjustment should be compiled on the basis of prospectively designed registry studies.
Similar content being viewed by others
References
Asher AL, McCormick PC, Selden NR, Ghogawala Z, McGirt MJ (2013) The National Neurosurgery Quality and Outcomes Database and NeuroPoint Alliance: rationale, development, and implementation. Neurosurg Focus 34:E2. https://doi.org/10.3171/2012.10.FOCUS12311
Asher AL, Parker SL, Rolston JD, Selden NR, McGirt MJ (2015) Using clinical registries to improve the quality of neurosurgical care. Neurosurg Clin N Am 26:253–263, ix-x. https://doi.org/10.1016/j.nec.2014.11.010
Buhr HJ, Hardt J, Klinger C, Seyfried F, Wiegering A, Dietrich A, Bartsch DK, Lorenz D, Post S, Germer CT, Keck T, Wellner U (2018) Quality indicators with reference values and threshold limits in general and visceral surgery : for obesity and metabolic, pancreatic, colon carcinoma and rectal carcinoma surgery. Chirurg 89:1–3. https://doi.org/10.1007/s00104-017-0562-5
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Cusimano MD, Pshonyak I, Lee MY, Ilie G (2017) A systematic review of 30-day readmission after cranial neurosurgery. J Neurosurg 127:342–352. https://doi.org/10.3171/2016.7.JNS152226
Dasenbrock HH, Liu KX, Devine CA, Chavakula V, Smith TR, Gormley WB, Dunn IF (2015) Length of hospital stay after craniotomy for tumor: a National Surgical Quality Improvement Program analysis. Neurosurg Focus 39:E12. https://doi.org/10.3171/2015.10.FOCUS15386
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity. A critical review of available methods. J Clin Epidemiol 56:221–229
Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE (2014) Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc 62:342–346. https://doi.org/10.1111/jgs.12635
Ghali WA, Quan H, Brant R (2001) Risk adjustment using administrative data: impact of a diagnosis-type indicator. J Gen Intern Med 16:519–524
Glassman S, Carreon LY, Andersen M, Asher A, Eiskjaer S, Gehrchen M, Imagama S, Ishii K, Kaito T, Matsuyama Y, Moridaira H, Mummaneni P, Shaffrey C, Matsumoto M (2017) Predictors of hospital readmission and surgical site infection in the United States, Denmark, and Japan: is risk stratification a universal language? Spine (Phila Pa 1976) 42:1311–1315. https://doi.org/10.1097/BRS.0000000000002082
Heller G (2008) Zur Messung und Darstellung von medizinischer Ergebnisqualität mit administrativen Routinedaten in Deutschland. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz:1173–1182
Iezzoni LI (1997) Assessing quality using administrative data. Ann Intern Med 127:666–674
Ingraham A, Nathens A, Peitzman A, Bode A, Dorlac G, Dorlac W, Miller P, Sadeghi M, Wasserman DD, Bilimoria K, American Association for the Surgery of Trauma Emergency General Surgery Quality Indicator Development Expert P (2017) Assessment of emergency general surgery care based on formally developed quality indicators. Surgery 162:397–407. https://doi.org/10.1016/j.surg.2017.03.025
Kennedy A, Bakir C, Brauer CA (2012) Quality indicators in pediatric orthopaedic surgery: a systematic review. Clin Orthop Relat Res 470:1124–1132. https://doi.org/10.1007/s11999-011-2060-2
Marventano S, Grosso G, Mistretta A, Bogusz-Czerniewicz M, Ferranti R, Nolfo F, Giorgianni G, Rametta S, Drago F, Basile F, Biondi A (2014) Evaluation of four comorbidity indices and Charlson comorbidity index adjustment for colorectal cancer patients. Int J Color Dis 29:1159–1169. https://doi.org/10.1007/s00384-014-1972-1
McGirt MJ, Speroff T, Dittus RS, Harrell FE Jr, Asher AL (2013) The National Neurosurgery Quality and Outcomes Database (N2QOD): general overview and pilot-year project description. Neurosurg Focus 34:E6. https://doi.org/10.3171/2012.10.FOCUS12297
McLaughlin N, Jin P, Martin NA (2015) Assessing early unplanned reoperations in neurosurgery: opportunities for quality improvement. J Neurosurg 123:198–205. https://doi.org/10.3171/2014.9.JNS14666
Moghavem N, Morrison D, Ratliff JK, Hernandez-Boussard T (2015) Cranial neurosurgical 30-day readmissions by clinical indication. J Neurosurg 123:189–197. https://doi.org/10.3171/2014.12.JNS14447
Nimptsch U (2016) Disease-specific trends of comorbidity coding and implications for risk adjustment in hospital administrative data. Health Serv Res 51:981–1001. https://doi.org/10.1111/1475-6773.12398
Schipmann S, Schwake M, Suero Molina E, Roeder N, Steudel WI, Warneke N, Stummer W (2017) Quality indicators in cranial neurosurgery: which are presently substantiated? A systematic review. World Neurosurg 104:104–112. https://doi.org/10.1016/j.wneu.2017.03.111
Schmidt HM, Gisbertz SS, Moons J, Rouvelas I, Kauppi J, Brown A, Asti E, Luyer M, Lagarde SM, Berlth F, Philippron A, Bruns C, Holscher A, Schneider PM, Raptis DA, van Berge Henegouwen MI, Nafteux P, Nilsson M, Rasanen J, Palazzo F, Rosato E, Mercer S, Bonavina L, Nieuwenhuijzen G, Wijnhoven BPL, Schroder W, Pattyn P, Grimminger PP, Gutschow CA (2017) Defining benchmarks for transthoracic esophagectomy: a multicenter analysis of Total minimally invasive esophagectomy in low risk patients. Ann Surg 266:814–821. https://doi.org/10.1097/SLA.0000000000002445
Shah MN, Stoev IT, Sanford DE, Gao F, Santiago P, Jaques DP, Dacey RG Jr (2013) Are readmission rates on a neurosurgical service indicators of quality of care? J Neurosurg 119:1043–1049. https://doi.org/10.3171/2013.3.JNS121769
Shih T, Dimick JB (2014) Reliability of readmission rates as a hospital quality measure in cardiac surgery. Ann Thorac Surg 97:1214–1218. https://doi.org/10.1016/j.athoracsur.2013.11.048
The Society of British Neurological Surgeons (2018) Neurosurgical National Audit Programme. Accessed 1407.2018 2018
Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK (2013) Variation in surgical-readmission rates and quality of hospital care. N Engl J Med 369:1134–1142. https://doi.org/10.1056/NEJMsa1303118
Wiegering A, Wellner U, Seyfried F, Hardt J, Klinger C, Buhr H, Post S (2017) MTL30 as surrogate parameter for quality of surgically treated diseases : establishment based on the StuDoQ register of the German Society for General and Visceral Surgery. Chirurg 88:977–982. https://doi.org/10.1007/s00104-017-0479-z
Yang CC, Chen PC, Hsu CW, Chang SL, Lee CC (2015) Validity of the age-adjusted charlson comorbidity index on clinical outcomes for patients with nasopharyngeal cancer post radiation treatment: a 5-year nationwide cohort study. PLoS One 10:e0117323. https://doi.org/10.1371/journal.pone.0117323
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the local ethic committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comments:
In a reasonably large sample of neurosurgical tumour cases, the authors calculated outcome parameters commonly regarded by politicians as indicators of quality of surgical care. In regression models, those outcome data were adjusted to individual risk factors, both endogenous in patients and including some complications during in-hospital stay. All parameters were retrieved from administrative data primarily collected for billing purposes. They found mainly a dependence of outcome on patient-clinical-complexity-level (PCCL), comorbidities, and male gender in pre-hospital data. As quality measures are increasingly discussed in many health systems (this data was obtained from Germany) and thus also may affect neurosurgical care, this is an important contribution, which approaches the very complex question of how to measure surgical quality with the data most easily accessible to date. As the authors point out, the approaches from different other countries such as the UK and the US cannot be directly transferred to the situation in Germany, e.g. due to a lack of patient registries. Obviously, for serious quality assessment and benchmarking, there is a need for nationwide patient registries. Thus, this notion and also the limitations have impact on neurosurgical practice and political attitudes despite different systems in different countries. Another important issue is that for example in gliomas, the extent of the surgical approach must be determined in individual cases in a complex trade-off between short-term outcome and long-term benefit. Therefore, "outcome Parameters" such as duration of hospital stay may not easily tell the whole truth. This paper is a valuable contribution to illustrate potential, but also limitations of such administrative data based approaches.
Georg Neuloh
Hans Clusmann
Aachen, Germany
This article is part of the Topical Collection on Neurosurgery general
Rights and permissions
About this article
Cite this article
Schipmann, S., Varghese, J., Brix, T. et al. Establishing risk-adjusted quality indicators in surgery using administrative data—an example from neurosurgery. Acta Neurochir 161, 1057–1065 (2019). https://doi.org/10.1007/s00701-018-03792-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-03792-2