Abstract
Background
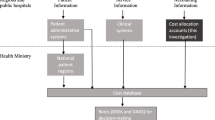
Economic evaluation of health technologies requires healthcare resources, procedures and services to be valued at their opportunity cost. In practice, many economic evaluation studies use official databases of hospital Diagnosis-Related Groups (DRGs) as inputs where unit costs are required. This study describes the available data on costs of hospital DRG from official, publicly available sources in nine European countries (England, France, Germany, Italy, Poland, Portugal, Slovenia, Spain and Sweden), critically examines and compares the methodologies used to construct these databases and comments on the appropriateness of such unit cost data for economic evaluation.
Methods
A standardized semi-structured questionnaire was developed in order to obtain both official publicly available sources of inpatient DRG databases and documents explaining the costing methodology used in calculation of unit costs available in those databases.
Results
England stands out as a benchmark in terms of good practice. Other countries face more challenges in one or more items, whether in documenting and auditing processes, guaranteeing methodological rigour, including all relevant economic items such as depreciation of buildings and equipment and capital costs, conducting the process annually and completely, publishing the costs as well as tariffs and recognising sampling uncertainty or variation.
Conclusion
Analysts should evaluate carefully whether DRG costs or tariffs published in each country are appropriate for use in economic evaluation.
Similar content being viewed by others

References
Fetter, R.B., Shin, Y., Freeman, J.L., Averill, R.F., Thompson, J.D.: Case mix definition by diagnosis-related groups. Med. Care. 18(2 Suppl), 1–53 (1980)
Feyrer, R., Rösch, J., Weyand, M., Kunzmann, U.: Cost unit accounting based on a clinical pathway: a practical tool for DRG implementation. Thorac. Cardiovasc. Surg. (2005). https://doi.org/10.1055/s-2005-865677
Kobel, C., Thuilliez, J., Bellanger, M., Pfeiffer, K-P.: DRG systems and similar patient classification systems in Europe. Diagnosis-related groups. In: Diagnosis-Related Groups in Europe. Moving Towards Transparency, Efficiency and Quality in Hospitals. European Observatory on Health Systems and Policies, pp. 37–58. Open University Press McGraw-Hill, Berkshire (2011)
Pirson, M., Schenker, L., Martins, D., Dung, D., Chalé, J.J., Leclercq, P.: What can we learn from international comparisons of costs by DRG? Eur. J. Heal. Econ. (2013). https://doi.org/10.1007/s10198-011-0373-4
Serdén, L., O’Reilly, J.: Patient classification and hospital reimbursement for inguinal hernia repair: a comparison across 11 European countries. Hernia (2014). https://doi.org/10.1007/s10029-013-1158-8
Escuela Andaluza de Salud Pública (EASP). European healthcare and social cost database. https://www.easp.es/Impact-Hta/default (2020). Accessed September 16, 2020.
Kalman, N., Hammill, B., Schulman, K., Shah, B.: Hospital overhead costs: the neglected driver of health care spending? J. Health Care Finance. 41, 4 (2015)
Tan SS, Serdén L, Geissler A, van Ineveld M, Redekop K, Heurgren M, et al. DRGs and cost accounting: which is driving which? In: Diagnosis-Related Groups in Europe. Moving Towards Transparency, Efficiency and Quality in Hospitals. European Observatory on Health Systems and Policies Series, Maidenhead, Open University Press McGraw-Hill, Berkshire (2011). pp 59–74.
Špacírová, Z., Epstein, D., García-Mochón, L., Rovira, J., Olry de Labry Lima, A., Espín, J.: A general framework for classifying costing methods for economic evaluation of health care. Eur. J. Heal. Econ. (2020). https://doi.org/10.1007/s10198-019-01157-9
Ergun, F.A., Agirbas, I., Kuzu, I.: Activity-based costing for pathology examinations and comparison with the current pricing system in Turkey. Turk. J. Pathol. (2013). https://doi.org/10.5146/tjpath.2013.01141
Mason A, Ward P, Street AD. England: the Healthcare Resource Group system. In: Diagnosis-Related Groups in Europe. Moving Towards Transparency, Efficiency and Quality in Hospitals. European Observatory on Health Systems and Policies Series, Maidenhead, Open University Press McGraw-Hill, Berkshire (2011). pp 197–220.
Busse, R., Schreyögg, J., Smith, P.C.: Variability in healthcare treatment costs amongst nine EU countries—results from the HealthBASKET project. Health Econ. (2008). https://doi.org/10.1002/hec.1330
EuroDRG. Diagnosis-Related Groups in Europe: Towards Efficiency and Quality. https://eurodrg.projects.tu-berlin.de/wiki/doku.php (2009). Accessed May 4, 2020.
join.me. https://www.join.me/. Accessed October 25, 2019.
NHS Improvement. 2019/20 National Tariff Payment System. https://improvement.nhs.uk/documents/4980/1920_National_Tariff_Payment_System.pdf (2020). Accessed September 5, 2020.
NHS England and NHS Improvement. 2020/21 National Tariff Payment System—a consultation notice. A guide to the market forces factor. https://improvement.nhs.uk/documents/6254/2021_Guide_to_the_market_forces_factor_consultation.pdf (2019). Accessed November 30, 2020.
Department of Health. NHS Costing Manual. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216427/dh_132398.pdf (2012). Accessed September 20, 2020.
NHS Improvement. Approved Costing Guidance. Costing glossary. https://www.england.nhs.uk/wp-content/uploads/2020/08/ACG_Glossary_FINAL.pdf (2020). Accessed October 12, 2020.
NHS Improvement. National cost collection guidance 2019. https://improvement.nhs.uk/documents/4883/National_cost_collections_19.pdf (2019). Accessed October 15, 2020.
NHS England and NHS Improvement. User guide: National Cost Collection 2018/19. https://www.england.nhs.uk/wp-content/uploads/2020/08/National_Cost_Collection_2018-19_A_Guide_to_using_the_data.pdf (2019). Accessed September 9, 2020.
Agence technique de l’information sur l’hospitalisation. Guide pratique d’utilisation du référentiel national de coûts SSR. Données ENC 2017. https://www.scansante.fr/sites/default/files/content/480/guide_pratique_ssr_2017.pdf (2017). Accessed May 19, 2020.
Chevreul, K., Berg Brigham, K., Durand-Zaleski, I., Hernández-Quevedo, C.: France. Health system review. Health Syst. Transition. 17(3), 1–218 (2015)
Gezelintzliche Krankeversicherung. Vereinbarung gemäß § 10 Abs. 9 KHEntgG für den Vereinbarungszeitraum 2020. https://www.gkv-spitzenverband.de/media/dokumente/krankenversicherung_1/krankenhaeuser/budgetverhandlungen/bundesbasisfallwert/KH_BBFW_2020_2019_11_25.pdf (2020). Accessed September 25, 2020.
Institut für das Entgeltsystem im Krankenhaus GmbH. Weiterentwicklung des G-DRG-Systems für das Jahr 2019. Klassifikation, Katalog und Bewertungsrelationen. https://www.g-drg.de/aG-DRG-System_2020/Abschlussbericht_zur_Weiterentwicklung_des_G-DRG-Systems_und_Report_Browser/Abschlussbericht_zur_Weiterentwicklung_des_aG-DRG-Systems_fuer_2020/Abschlussbericht_zur_Weiterentwicklung_des_G-DRG-Systems_fuer_2020 (2020). Accessed June 3, 2020.
Quatidiano sanità. Relazione tecnica. http://www.quotidianosanita.it/allegati/allegato5477154.pdf Accessed March 9, 2020.
Agencja Oceny Techonologii Medycznych i Taryfikacji. Załącznik Nr 2. Zasady analizy danych kosztowych uzyskanych od świadczeniodawców. https://www2.aotm.gov.pl/wp-content/uploads/2016/08/WT_541_5_2016_witrektomia_Zal_2_Zasady_analizy_danych_kosztowych.pdf (2016). Accessed June 4, 2020.
Ministério da Saúde & Instituto de Gestão Informática e Financeira da Saúde. Plano de Contabilidade Analítica dos Hospitais—3a Edição. https://www2.acss.min-saude.pt/Portals/0/DownloadsPublicacoes/SNS/Info_gestao/PCAH_3Edicao.pdf (2007). Accessed June 14, 2020.
Zavod za zdravstveno zavarovanje Slovenije. Splošni dogovor za pogodbeno leto 2019. Pril I Kalkulacije Za Plan Financ Programov Zdr Storit 2019. https://www.zzzs.si/Zzzs/info/egradiva.nsf/o/37D1B2F27B0EC343C12583B7002DAF04?OpenDocument (2009). Accessed November 20, 2020.
Zavod za zdravstveno zavarovanje Slovenije. Ralizacija SPP po izvajalcih 1–12 2020. https://partner.zzzs.si/wps/portal/portali/aizv/zdravstvene_storitve/plan_in_realizacija/podatki_o_planu_in_realizaciji_zdrav_storitve (2020). Accessed December 31, 2020.
Ministerio de Sanidad Consumo y Bienestar. Estimación de pesos y costes de los procesos hospitalarios en el Sistema Nacional de Salud: metodología y principales resultados. https://www.mscbs.gob.es/fr/estadEstudios/estadisticas/docs/CMBD/Inf_proc_estim_cost_hosp_SNS2017.pdf (2017). Accessed May 12, 2020.
Ministerio de Sanidad, Consumo y Bienestar Social. Recomendaciones para la obtención homogénea de costes de hospitalización en el SNS. https://www.mscbs.gob.es/estadEstudios/estadisticas/docs/REC_OBT_HOM_COST_HOSPIT_SNS.pdf (2013). Accessed March 5, 2020.
Sveriges Kommuner och Landsting. Nationella KPP-principer. VERSION 3. KOSTNAD PER PATIENT. https://vardgivarguiden.se/globalassets/administration/verksamhetsadministration/rapportera/vardinformatik/klassifikationer/nationella-kpp--principer-version-3.pdf (2015). Accessed January 20, 2021.
Socialstyrelsen 2021. Arbetsprocessen för nationella prospektiva vikter—Uppdatering inför 2021. https://www.socialstyrelsen.se/utveckla-verksamhet/e-halsa/klassificering-och-koder/drg/viktlistor/ (2021). Accessed January 20, 2021.
NHS Improvement. National Schedule of Reference Costs: Year 2017–2018. https://webarchive.nationalarchives.gov.uk/ukgwa/20200501111106/https:/improvement.nhs.uk/resources/reference-costs/ (2018). Accessed January 9, 2019.
NHS Improvement. Annex A: The national tariff workbook. https://improvement.nhs.uk/resources/national-tariff/#h2-201920-national-tariff-payment-system (2019). Accessed January 14, 2020.
NHS Improvement. 2019–2020 Reference Costs Collection. https://digital.nhs.uk/data-andinformation/data-collections-and-data-sets/data-collections/reference-costs (2020). Accessed November 7, 2020.
ScanSanté. ENC MCO. https://www.scansante.fr/applications/enc-mco (2019). Accessed September 9, 2020.
Agence Technique de l’information sur l’hospitalisation. Tarifs MCO et HAD. https://www.atih.sante.fr/tarifs-mco-et-had (2020). Accessed February 6, 2020.
Deutsche Krankenhaus Gesellschaft. Fallpauschalen-Katalog. https://www.dkgev.de/fileadmin/default/Fallpauschalenkatalog_2019_180928.pdf (2019). Accessed May 31, 2019.
Ministero della Salute. Decreto legislativo 30 dicembre 1992, n. 502. Riordino della disciplina in materia sanitaria, a norma dell’articolo 1 della legge 23 ottobre 1992, n. 421. Art. 8-sexies. (Remunerazione). https://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=13209&articolo=30 (1992). Accessed March 9, 2020.
Narodowy Fundusz Zdrowia. Zarządzenie Nr 38/2019/DSOZ Prezesa Narodowego Funduszu Zdrowia z dnia 29 marca 2019 r. w sprawie określenia warunków zawierania i realizacji umów w rodzaju leczenie szpitalne oraz leczenie szpitalne - świadczenia wysokospecjalistyczne. https://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-382019dsoz,6906.html (2019). Accessed April 17, 2020.
Serviço Nacional de Saúde. Tabela de preços do SNS 2018. Portaria no 254/2018, de 7 de setembro. http://www.acss.min-saude.pt/category/acss_pt/tabelas-e-impressos/ (2018). Accessed February 24, 2020.
Junta de Aragón. ORDEN SAN/1221/2017, de 21 de julio, por la que se establecen los precios y tarifas máximas aplicables en la prestación de servicios sanitarios con medios ajenos al Sistema de Salud de Aragón. http://www.boa.aragon.es/cgi-bin/EBOA/BRSCGI?CMD=VEROBJ&MLKOB=977342223030 (2017). Accessed February 27, 2020.
Junta de Andalucí. Boletín Oficial de la Junta de Andalucía n°210. Orden de 14 de octubre de 2005, por la que se fijan los precios públicos de los servicios sanitarios prestados por Centros dependientes del Sistema Sanitario Público de Andalucía. https://juntadeandalucia.es/boja/2005/210/boletin.210.pdf (2005). Accessed July 23, 2020.
Xunta de Galicia. DECRETO 56/2014, de 30 de abril, por el que se establecen las tarifas de los servicios sanitarios prestados en los centros dependientes del Servicio Gallego de Salud y en las fundaciones públicas sanitarias. https://www.xunta.gal/dog/Publicados/2017/20170714/AnuncioG0164-100717-0001_es.html (2017). Accessed February 26, 2020.
Comunidad de Madrid. ORDEN 727/2017, de 7 de agosto, del Consejero de Sanidad, por la que se fijan los precios públicos por la prestación de los servicios y actividades de naturaleza sanitaria de la red de centros de la Comunidad de Madrid. Comunidad de Madrid. http://www.madrid.org/wleg_pub/secure/quienesSomos/quienesSomos.jsf?id=2 (2017). Accessed February 26, 2020.
Södra Sjukvårdsregionen. Regionala priser och ersättningar för södra sjukvårdsregionen. https://sodrasjukvardsregionen.se/download/regionala-priser-och-ersattningar-for-sodra-sjukvardsregionen-2020/ (2020). Accessed April 14, 2020.
Sydöstra sjukvårdsregionen. Priser och ersättningar för Sydöstra sjukvårdsregionen. https://plus.rjl.se/info_files/infosida44878/prislista_2020_version4_0.pdf (2020). Accessed April 14, 2020.
NHS Digital. Patient Level Information and Costing System (PLICS) Data Collections. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/patient-level-information-and-costing-system-plics-data-collections (2020). Accessed November 10, 2020.
Department of Health & Social Care. Group Accounting Manual 2017–18. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/696294/2017-18_DH_GAM_-_March_18.pdf (2018). Accessed February 20, 2019.
Turner, H.C., Lauer, J.A., Tran, B.X., Teerawattananon, Y., Jit, M.: Adjusting for inflation and currency changes within health economic studies. Value Heal. (2019). https://doi.org/10.1016/j.jval.2019.03.021
Gold, M., Siegel, J., Russell, L., Weinstein, M.: Cost-Effectiveness in Health and Medicine. Oxford University Press, New York (1996)
Acknowledgements
The authors are very thankful to Erica Visintin, Isabelle Durand-Zaleski, Meryl Darlington, Wolfgang Greiner, Elena Nicod, Michela Meregaglia, Marco Marchetti, Aneta Lipinska, Monica Oliveira, Valentina Katka Rupel, Douglas Loundin and Lars-Åke Levin, for completion of the questionnaire or provision of documentation on costing methodology. The opinions expressed in this article are entirely those of the authors.
Funding
This study has received funding from the European Union’s Horizon 2020 research and innovation programme under Grant agreement no. 779312.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Špacírová, Z., Epstein, D. & Espín, J. Are costs derived from diagnosis-related groups suitable for use in economic evaluations? A comparison across nine European countries in the European Healthcare and Social Cost Database. Eur J Health Econ 23, 1563–1575 (2022). https://doi.org/10.1007/s10198-022-01444-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-022-01444-y