Abstract
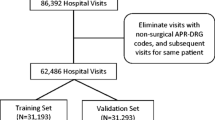
The aims of this study were to assess All-Patient Refined Diagnosis-Related Groups’ (APR-DRG) Severity of Illness (SOI) and Risk of Mortality (ROM) as predictors of in-hospital mortality, comparing with Charlson Comorbidity Index (CCI) and Elixhauser Comorbidity Index (ECI) scores. We performed a retrospective observational study using mainland Portuguese public hospitalizations of adult patients from 2011 to 2016. Model discrimination (C-statistic/ area under the curve) and goodness-of-fit (R-squared) were calculated. Our results comprised 4,176,142 hospitalizations with 5.9% in-hospital deaths. Compared to the CCI and ECI models, the model considering SOI, age and sex showed a statistically significantly higher discrimination in 49.6% (132 out of 266) of APR-DRGs, while in the model with ROM that happened in 33.5% of APR-DRGs. Between these two models, SOI was the best performer for nearly 20% of APR-DRGs. Some particular APR-DRGs have showed good discrimination (e.g. related to burns, viral meningitis or specific transplants). In conclusion, SOI or ROM, combined with age and sex, perform better than more widely used comorbidity indices. Despite ROM being the only score specifically designed for in-hospital mortality prediction, SOI performed better. These findings can be helpful for hospital or organizational models benchmarking or epidemiological analysis.


Similar content being viewed by others
References
Minne L, Ludikhuize J, de Rooij SE, Abu-Hanna A. Characterizing predictive models of mortality for older adults and their validation for use in clinical practice. J Am Geriatr Soc. 2011 Jun;59(6):1110-5.
Larsson J, Itenov TS, Bestle MH. Risk prediction models for mortality in patients with ventilator-associated pneumonia: A systematic review and meta-analysis. J Crit Care. 2017 Feb;37:112-118.
Sharma, N., Schwendimann, R., Endrich, O., Ausserhofer, D., & Simon, M. (2021). Comparing Charlson and Elixhauser comorbidity indices with different weightings to predict in-hospital mortality: an analysis of national inpatient data. BMC health services research, 21(1), 13.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383.
Elixhauser A, Steiner C, Robert Harris D, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998; 36: 8–27.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130–1139.
Quan H, Bing L, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011; 173: 676–682.
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 2009; 47: 626–633.
Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data. Med Care 2017; 55: 698–705.
Schneeweiss S, Wang PS, Avorn J, Glynn RJ. Improved comorbidity adjustment for predicting mortality in Medicare populations. Health Serv Res. 2003; 38(4):1103–1120.
Thompson NR, Fan Y, Dalton JE, Jehi L, Rosenbaum BP, Vadera S, Griffith SD. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care. 2015; 53(4):374–379.
Fetter RB, Thompson JD, Mills RE. A system for cost and reimbursement control in hospitals. Yale J Biol Med 1976; 49: 123–136.
Busse R, Geissler A, Quentin W, et al. Diagnosis Related Groups in Europe. Moving towards Transparency, Efficiency and Quality in Hospitals. Copenhagen: Open University Press. 2011.
Schreyogg J, Stargardt T, Tiemann O, Busse R. Methods to determine reimbursement rates for diagnosis related groups (DRG): a comparison of nine European countries. Health Care Management Sci 2006; 9(3): 215–223.
Mathauer I, Wittenbecher F. Hospital payment systems based on diagnosis-related groups: Experiences in low- and middle-income countries. Bull World Health Organ 2013; 91: 746–756.
Mihailovic, N., Kocic, S., & Jakovljevic, M. Review of Diagnosis-Related Group-Based Financing of Hospital Care. Health services research and managerial epidemiology, 3, 2333392816647892. 2016.
Averill R, Goldfield N, et al. All Patient Refined Diagnosis Related Groups (APR-DRGs) Version 31.0: Methodology Overview [Internet]. Available from: https://hcup-us.ahrq.gov/db/nation/nis/grp031_aprdrg_meth_ovrview.pdf [Accessed in Jun 15 2021].
Dewilde, S, Annemans, L, Pincé, H, Thijs, V. Hospital financing of ischemic stroke: determinants of funding and usefulness of DRG subcategories based on severity of illness. BMC Health Serv Res. 2018; 18(1): 356.
Nante N, De Marco MF, Balzi D, Addari P, Buiatti E. Prediction of mortality for congestive heart failure patients: results from different wards of an Italian teaching hospital. Eur J Epidemiol. 2000; 16: 1017–21.
Iezzoni LI, Shwartz M, Ash AS, Mackiernan YD. Predicting in-hospital mortality for stroke patients: results differ across severity-measurement methods. Med Decis Making. 1996; 16(4): 348–356.
Baram D, Daroowalla F, Garcia R, Zhang G, Chen JJ, Healy E, Riaz SA, Richman P. Use of the All Patient Refined-Diagnosis Related Group (APR-DRG) Risk of Mortality Score as a Severity Adjustor in the Medical ICU. Clin Med Circ Respirat Pulm Med. 2008; 2: 19–25.
McCormick PJ, Lin HM, Deiner SG, Levin MA. Validation of the All Patient Refined Diagnosis Related Group (APR-DRG) Risk of Mortality and Severity of Illness Modifiers as a Measure of Perioperative Risk. J Med Syst. 2018; 42(5): 81.
Romano PS, Chan BK. Risk-adjusting acute myocardial infarction mortality: are APR-DRGs the right tool? Health Serv Res. 2000 Mar;34(7):1469–89.
Liu J, Larson E, Hessels A, Cohen B, Zachariah P, Caplan D, Shang J. Comparison of Measures to Predict Mortality and Length of Stay in Hospitalized Patients. Nurs Res. 2019; 68(3): 200–209.
DiCiccio TJ and Efron B. Bootstrap Confidence Intervals. Statistical Science 1996; 11: 189.
Souza J, Santos JV, Canedo VB, Betanzos A, Alves D, Freitas A. Importance of coding co-morbidities for APR-DRG assignment: Focus on cardiovascular and respiratory diseases. Health Inf Manag 2020; 49: 47–57.
Bahlis LF, Diogo LP, Fuchs SC. Charlson Comorbidity Index and other predictors of in-hospital mortality among adults with community-acquired pneumonia. J Bras Pneumol. 2021; 47(1): e20200257.
Christensen S, Johansen MB, Christiansen CF, Jensen R, Lemeshow S. Comparison of Charlson comorbidity index with SAPS and APACHE scores for prediction of mortality following intensive care. Clin Epidemiol. 2011; 3: 203–211.
Quach S, Hennessy DA, Faris P, Fong A, Quan H, Doig C. A comparison between the APACHE II and Charlson Index Score for predicting hospital mortality in critically ill patients. BMC Health Serv Res. 2009; 9: 129.
Bennett CE, Wright RS, Jentzer J, Gajic O, Murphree DH, Murphy JG, Mankad SV, Wiley BM, Bell MR, Barsness GW. Severity of illness assessment with application of the APACHE IV predicted mortality and outcome trends analysis in an academic cardiac intensive care unit. J Crit Care. 2019; 50: 242–246.
Wang H, Johnson C, Robinson RD, Nejtek VA, Schrader CD, Leuck J, Umejiego J, Trop A, Delaney KA, Zenarosa NR. Roles of disease severity and post-discharge outpatient visits as predictors of hospital readmissions. BMC Health Serv Res. 2016; 16(1): 564.
Jokinen JJ. Why do we have to predict mortality rates? Acta Anaesthesiol Scand. 2011; 55(3): 255–256.
Mascha EJ, Mazo V. Predicting In-hospital Postoperative Mortality for the Practitioner: Beyond the Numbers. Anesthesiology. 2016; 124(3): 523–525.
El Amrani M, Clement G, Lenne X, Rogosnitzky M, Theis D, Pruvot FR, Zerbib P. The Impact of Hospital Volume and Charlson Score on Postoperative Mortality of Proctectomy for Rectal Cancer: A Nationwide Study of 45,569 Patients. Ann Surg. 2018; 268(5): 854–860.
Jarman B, Pieter D, van der Veen AA, Kool RB, Aylin P, Bottle A, Westert GP, Jones S. The hospital standardised mortality ratio: a powerful tool for Dutch hospitals to assess their quality of care? Qual Saf Health Care. 2010; 19(1): 9–13.
Bhandari S, Abdul MKM, Hollabaugh W, Sharma K, Evans DB, Guda N. Decreased trend in hospital mortality from pancreatic cancer despite increase in number of hospital admissions. PLoS One. 2018; 13(7): e0199909.
Stavem K, Hoel H, Skjaker SA, Haagensen R. Charlson comorbidity index derived from chart review or administrative data: agreement and prediction of mortality in intensive care patients. Clin Epidemiol. 2017; 9: 311–320.
Weir RE Jr, Lyttle CS, Meltzer DO, Dong TS, Ruhnke GW. The Relative Ability of Comorbidity Ascertainment Methodologies to Predict In-Hospital Mortality Among Hospitalized Community-acquired Pneumonia Patients. Med Care. 2018; 56(11): 950–955.
Peng M, Southern DA, Williamson T, Quan H. Under-coding of secondary conditions in coded hospital health data: Impact of co-existing conditions, death status and number of codes in a record. Health Informatics J. 2017; 23(4): 260–267.
Ramalho A., Souza J., Freitas A. The Use of Artificial Intelligence for Clinical Coding Automation: A Bibliometric Analysis. In: Dong Y., Herrera-Viedma E., Matsui K., Omatsu S., González Briones A., Rodríguez González S. (eds) Distributed Computing and Artificial Intelligence, 17th International Conference. DCAI 2020. Advances in Intelligent Systems and Computing, vol 1237. Springer, Cham. 2021.
Stanfill MH, Williams M, Fenton SH, Jenders RA, Hersh WR. A systematic literature review of automated clinical coding and classification systems. J Am Med Inform Assoc. 2010; 17(6): 646–651.
Catling F, Spithourakis GP, Riedel S. Towards automated clinical coding. Int J Med Inform. 2018; 120: 50–61.
Mpanya D, Celik T, Klug E, Ntsinjana H. Machine learning and statistical methods for predicting mortality in heart failure. Heart Fail Rev. 2021 May;26(3):545-552. https://doi.org/10.1007/s10741-020-10052-y. Epub 2020 Nov 9. PMID: 33169338.
Weissman GE, Hubbard RA, Ungar LH, Harhay MO, Greene CS, Himes BE, Halpern SD. Inclusion of Unstructured Clinical Text Improves Early Prediction of Death or Prolonged ICU Stay. Crit Care Med. 2018; 46(7): 1125–1132.
Rajkomar A, Oren E, Chen K, Dai AM, Hajaj N, Hardt M, Liu PJ, Liu X, Marcus J, Sun M, Sundberg P, Yee H, Zhang K, Zhang Y, Flores G, Duggan GE, Irvine J, Le Q, Litsch K, Mossin A, Tansuwan J, Wang D, Wexler J, Wilson J, Ludwig D, Volchenboum SL, Chou K, Pearson M, Madabushi S, Shah NH, Butte AJ, Howell MD, Cui C, Corrado GS, Dean J. Scalable and accurate deep learning with electronic health records. NPJ Digit Med. 2018; 1: 18.
Syed M, Syed S, Sexton K, Greer ML, Zozus M, Bhattacharyya S, Syed F, Prior F. Deep Learning Methods to Predict Mortality in COVID-19 Patients: A Rapid Scoping Review. Stud Health Technol Inform. 2021; 281: 799–803.
Alonso V, Santos JV, Pinto M, Ferreira J, Lema I, Lopes F, Freitas A. Health records as the basis of clinical coding: Is the quality adequate? A qualitative study of medical coders' perceptions. Health Inf Manag. 2020; 49(1): 28–37.
Santos JV, Novo R, Souza J, Lopes F, Freitas A. Transition from ICD-9-CM to ICD-10-CM/PCS in Portugal: An heterogeneous implementation with potential data implications. Health Inf Manag. 2021 [epub ahead of print].
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Health Policy
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Santos, J.V., Viana, J., Pinto, C. et al. All Patient Refined-Diagnosis Related Groups’ (APR-DRGs) Severity of Illness and Risk of Mortality as predictors of in-hospital mortality. J Med Syst 46, 37 (2022). https://doi.org/10.1007/s10916-022-01805-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-022-01805-3