Abstract
Background
With modern intensive care medicine, even older patients and those with pre-existing conditions can survive critical illnesses and major operations; however, unreflected application of intensive care treatment might lead to a state called chronic critical illness. Today, withholding treatment and/or treatment withdrawal precede many deaths in the intensice care unit (ICU). We looked at changes in measures at the end of life and withholding or withdrawal of treatment in the ICU of a German tertiary hospital in 2017/2018 compared to 2011/2012.
Methods
In this retrospective explorative study, we analyzed end of life practices in adult patients who died in an intermediate care unit (IMC)/ICU of Klinikum Hanau in 2017/2018. We compared these data with data from the same hospital in 2011/2012
Results
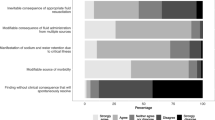
Of the 1246 adult patients who died in Klinikum Hanau in 2017/2018, 433 (35%) died in an ICU or IMC unit. Deceased ICU patients were 74.0 ± 12.5 years and 86.6% were older than 60 years. At least one life-sustaining measure was withheld in 278 (76.2%) and withdrawn in 159 (46.3%) of patients. More than three quarters of patients (n = 276, 75.6%) had a do not resuscitate (DNR) order and in about half of the patients invasive ventilation (n = 175, 49.9%) or renal replacement therapy (n = 191, 52.3%) was limited. In 113 patients (31.0%) catecholamine treatment was withdrawn, in 72 (19.7%) patients invasive ventilation and in 49 (13.4%) patients renal replacement therapy. Compared to 2011/2012, we saw an increase by ~15% (absolute increase) in withholding and withdrawal of treatment and observed an effect of documents like advance directive or healthcare proxy.
Conclusion
In 76.2% of deceased ICU patients withholding treatment and in 43.6% treatment withdrawal preceded death. Compared to 2011/2012 treatment was withheld or withdrawn more often. Compared to 2011/2012, we saw an increase (~15% absolute) in withholding and withdrawal of treatment. After withholding or withdrawal of treatment, most patients died within 3 and 2 days, respectively.
Zusammenfassung
Hintergrund
Mittels moderner intensivmedizinischer Methoden können auch ältere Menschen und Menschen mit erheblichen Vorerkrankungen größere Operationen und kritische Erkrankungen überleben. Die unkritische Anwendung intensivmedizinischer Maßnahmen kann jedoch auch zu einem Zustand führen, der als chronische kritische Erkrankung bezeichnet wird. Da wahrscheinlich vielen Todesfällen auf der Intensivstation Therapiebegrenzungen oder -abbrüche vorangehen, haben wir Akten von Todesfällen der Jahre 2017/2018 angesehen und mit Daten aus den Jahren 2011/2012 verglichen.
Material und Methoden
In dieser retrospektiven explorativen Arbeit haben wir Todesfälle auf den Intensiv‑/Intermediate-Care-Stationen (chirurgisch/interdisziplinär und konservativ) des Klinikum Hanau in den Jahren 2017/2018 bzgl. Therapiebegrenzungen und Therapieabbrüchen untersucht und diese den Daten aus 2011/2012 gegenübergestellt.
Ergebnisse
In den Jahren 2017/2018 sind 1246 Patienten im Klinikum Hanau verstorben. Davon starben 433 (35 %) auf einer Intensiv‑/Intermediate-Care-Station. Die verstorbenen Intensivpatienten waren im Mittel 74,0 ± 12,5 Jahre alt und 86,6 % waren älter als 60 Jahre. Bei 278 Patienten (76,2 %) wurde mindestens eine Maßnahme begrenzt, bei 159 (46,3 %) mindestens eine Maßnahme abgebrochen. Mehr als drei Viertel aller Patienten (276, 75,6 %) hatte eine „Do-not-resuscitate“(DNR)-Anordnung, und bei über der Hälfte der Verstorbenen wurde die invasive Beatmung (n = 175, 49,9 %) oder eine Nierenersatztherapie (n = 191, 52,3 %) begrenzt. Bei 113 Patienten (31,0 %) wurde die Katecholamintherapie, bei 72 (19,7 %) Patienten die invasive Beatmung und bei 49 (13,4 %) Patienten eine Nierenersatztherapie abgebrochen. Sowohl bei den Therapiebegrenzungen wie auch den -abbrüchen sind die Zahlen im Vergleich zu 2011/2012 um ca. absolute 15 % (absolute Zunahme) gestiegen wobei ein Effekt von Vorsorgedokumenten zu erkennen war.
Diskussion
Bei 76,2 % der verstorbenen Intensivpatienten wurde eine Therapie begrenzt und bei 43,6 % abgebrochen. Im Vergleich zu 2011/2012 sind mehr Therapien begrenzt und abgebrochen worden. Nach Begrenzung oder Abbruch einer Therapie sind die meisten Patienten innerhalb von 3 bzw. 2 Tagen verstorben.

Similar content being viewed by others
Abbreviations
- BPM:
-
Blood pressure measurement
- CPR:
-
Cardiopulmonary resuscitation
- CVL:
-
Central venous line
- DNR:
-
Do not resuscitate
- DRG:
-
German diagnosis-related group
- ICU:
-
Intensive care unit
- IMC:
-
Intermediate care unit
- IV:
-
Invasive ventilation
- NGT:
-
Nasogastral tube
- NIV:
-
Noninvasive ventilation
- RRT:
-
Renal replacement therapy
- PRG/PEJ:
-
Percutaneous endoscopic gastrostomy/jejunostomy
References
Garrett JM, Harris RP, Norburn JK, Patrick DL, Danis M (1993) Life-sustaining treatments during terminal illness: who wants what? J Gen Intern Med 8:361–368
Hillman K, Athari F, Forero R (2018) States worse than death. Curr Opin Crit Care 24:415–420. https://doi.org/10.1097/MCC.0000000000000529
Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, Rubenfeld GD (2004) Use of intensive care at the end of life in the United States: an epidemiologic. Crit Care Med 32:638–643
Ely EW, Azoulay E, Sprung CL (2019) Eight things we would never do regarding end-of-life care in the ICU. Intensive Care Med. https://doi.org/10.1007/s00134-019-05562-9
Mosenthal AC, Murphy PA, Barker LK, Lavery R, Retano A, Livingston DH (2008) Changing the culture around end-of-life care in the trauma intensive care unit. J Trauma 64:1587–1593. https://doi.org/10.1097/TA.0b013e318174f112
Cardona-Morrell M, Kim J, Turner RM, Anstey M, Mitchell IA, Hillman K (2016) Non-beneficial treatments in hospital at the end of life: a systematic review on extent of the problem. Int J Qual Health Care 28:456–469. https://doi.org/10.1093/intqhc/mzw060
Wiesing U, Jox RJ, Hessler H‑J, Borasio GD (2010) A new law on advance directives in Germany. J Med Ethics 36:779–783. https://doi.org/10.1136/jme.2010.036376
Mentzelopoulos SD, Couper K, Van de Voorde P, Druwé P, Blom M, Perkins GD et al (2021) European resuscitation council guidelines 2021: ethics of resuscitation and end of life decisions. Resuscitation 161:408–432. https://doi.org/10.1016/j.resuscitation.2021.02.017
Neitzke G, Burchardi H, Duttge G, Hartog C, Erchinger R, Gretenkort P et al (2016) Limits of the meaningfulness of intensive care medicine: position paper of the ethics section of DIVI. Med Klin Intensivmed Notfmed. https://doi.org/10.1007/s00063-016-0202-8
Ay E, Weigand MA, Röhrig R, Gruss M (2020) Dying in the intensive care unit (ICU): a retrospective descriptive analysis of deaths in the ICU in a communal tertiary hospital in Germany. Anesthesiol Res Pract 2020:2356019. https://doi.org/10.1155/2020/2356019
Sprung CL, Cohen SL, Sjokvist P, Baras M, Bulow H‑H, Hovilehto S et al (2003) End-of-life practices in European intensive care units: the ethicus study. JAMA 290:790–797. https://doi.org/10.1001/jama.290.6.790
Sprung CL, Ricou B, Hartog CS, Maia P, Mentzelopoulos SD, Weiss M et al (2019) Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA. https://doi.org/10.1001/jama.2019.14608
Graw JA, Spies CD, Kork F, Wernecke K‑D, Braun J‑P (2015) End-of-life decisions in intensive care medicine-shared decision-making and intensive care unit length of stay. World J Surg 39:644–651. https://doi.org/10.1007/s00268-014-2884-5
Graw JA, Spies CD, Wernecke K‑D, Braun J‑P (2012) Managing end-of-life decision making in intensive care medicine—a perspective from Charité Hospital, Germany. PLoS One 7:e46446. https://doi.org/10.1371/journal.pone.0046446
Lee SI, Hong KS, Park J, Lee Y‑J (2020) Decision-making regarding withdrawal of life-sustaining treatment and the role of intensivists in the intensive care unit: a single-center study. Acute Crit Care 35:179–188. https://doi.org/10.4266/acc.2020.00136
Robert R, Le Gouge A, Kentish-Barnes N, Adda M, Audibert J, Barbier F et al (2020) Sedation practice and discomfort during withdrawal of mechanical ventilation in critically ill patients at end-of-life: a post-hoc analysis of a multicenter study. Intensive Care Med 46:1194–1203. https://doi.org/10.1007/s00134-020-05930-w
Neitzke G, Böll B, Burchardi H, Dannenberg K, Duttge G, Erchinger R et al (2017) Dokumentation der Therapiebegrenzung : Empfehlung der Sektion Ethik der Deutschen Interdisziplinären Vereinigung für Intensiv- und Notfallmedizin (DIVI) unter Mitarbeit der Sektion Ethik der Deutschen Gesellschaft für Internistische Intensivmedizin und Notfallmedizin (DGIIN). Med Klin Intensivmed Notfmed 112:527–530. https://doi.org/10.1007/s00063-017-0321-x
Gruß M, Salomon F (2016) Autonomy and welfare in intensive care medicine : practical approach in difficult situations. Anaesthesist 65:875–888. https://doi.org/10.1007/s00101-016-0222-z
InEK GmbH – Institut für das Entgeltsystem im Krankenhaus (2021) German diagnosis related group system. https://www.g-drg.de/. Accessed 8 Apr 2021
Dos Anjos CS, Borges RMC, Chaves AC, de Souza Lima AC, Pereira MBM, Gasparoto ML et al (2019) Religion as a determining factor for invasive care among physicians in end-of-life patients. Support Care Cancer. https://doi.org/10.1007/s00520-019-04846-6
Hartog CS, Hoffmann F, Mikolajetz A, Schröder S, Michalsen A, Dey K et al (2018) Non-beneficial therapy and emotional exhaustion in end-of-life care : results of a survey among intensive care unit personnel. [non-beneficial therapy and emotional exhaustion in end-of-life care : results of a survey among intensive care unit personnel]. Anaesthesist 67:850–858. https://doi.org/10.1007/s00101-018-0485-7
Revon-Rivière G, Pauly V, Baumstarck K, Bernard C, André N, Gentet J‑C et al (2019) High-intensity end-of-life care among children, adolescents, and young adults with cancer who die in the hospital: a population-based study from the French national hospital database. Cancer. https://doi.org/10.1002/cncr.32035
Fleischmann-Struzek C, Mikolajetz A, Reinhart K, Curtis RJ, Haase U, Thomas-Rüddel D et al (2019) Hospitalization and intensive therapy at the end of life. Dtsch Arztebl Int 116:653–660. https://doi.org/10.3238/arztebl.2019.0653
Veshi D, Neitzke G (2016) Council of Europe. Med Law Int 16:94–102. https://doi.org/10.1177/0968533216659785
Azoulay E, Timsit JF, Sprung CL, Soares M, Rusinova K, Lafabrie A et al (2009) Prevalence and factors of intensive care unit conflicts: the conflicus study. Am J Respir Crit Care Med 180:853–860
Bruno RR, Wernly B, Beil M, Muessig JM, Rahmel T, Graf T et al (2020) Therapy limitation in octogenarians in German intensive care units is associated with a longer length of stay and increased 30 days mortality: a prospective multicenter study. J Crit Care 60:58–63. https://doi.org/10.1016/j.jcrc.2020.07.024
Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD et al (2008) Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American college corrected of critical care medicine. Crit Care Med 36:953–963. https://doi.org/10.1097/CCM.0B013E3181659096
Lustbader D, Pekmezaris R, Frankenthaler M, Walia R, Smith F, Hussain E et al (2011) Palliative medicine consultation impacts DNR designation and length of stay for terminal medical MICU patients. Palliat Support Care 9:401–406. https://doi.org/10.1017/S1478951511000423
Hua MS, Li G, Blinderman CD, Wunsch H (2014) Estimates of the need for palliative care consultation across united states intensive care units using a trigger-based model. Am J Respir Crit Care Med 189:428–436. https://doi.org/10.1164/rccm.201307-1229OC
Rady MY, Johnson DJ (2004) Admission to intensive care unit at the end-of-life: is it an informed decision? Palliat Med 18:705–711
Acknowledgements
We thank Mrs. Esma Ay for introducing IS in analysis of patients’ charts and many helpful discussions about end-of-life decisions.
Funding
None; this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
IS analyzed the patients’ charts, made the figure and tables. MAW had the idea for the study and made substantial reviews. MHG supported the study design and calculated the statistical analysis. MG had the idea for the study, planned it, carried it out and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
I. Schulmeyer, M.A. Weigand, M. Heinzel-Gutenbrunner and M. Gruss declare that they have no competing interests.
Ethical approval was given before analyzing data by the Medical Council (Landesärztekammer) Hesse (AZ 2019-1244-evBO, 28.11.2019, second period and FF 131/2013, 23.01.2014, first period).
Additional information
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Schulmeyer, I., Weigand, M.A., Heinzel-Gutenbrunner, M. et al. Dying in the ICU. Anaesthesiologie 71, 930–940 (2022). https://doi.org/10.1007/s00101-022-01127-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-022-01127-6